Sensation Preserving Mastectomies
After Anne Peled, M.D. was diagnosed with breast cancer at 37, she carefully weighed all of her options and opted for a lumpectomy rather than a mastectomy, in large part because of having to face the prospect of losing sensation if she opted for a mastectomy and implant reconstruction. As a result of this experience, she and her husband Dr. Ziv Peled (a peripheral nerve and plastic surgeon) began to discuss ways in which they could use their combined, highly specialized skill sets to preserve and restore sensation during mastectomies and implant breast reconstruction. They are now performing sensation preserving mastectomy procedures as well as nipple-sparing mastectomies to patients. They have developed a technique for preserving and grafting nerves that are typically injured during mastectomy. This approach is often performed in combination with nipple-sparing mastectomy and implant breast reconstruction.

Drs. anne and ziv peled speak about sensation preserving mastectomies
Who is a candidate for Sensation Preserving Mastectomy?
Sensation-preserving mastectomies can be offered to those who are diagnosed with breast cancer or those who are at high risk for future breast cancer and are considering prophylactic mastectomy. Sensation preservation at the time of mastectomy involves saving nerves when oncologically safe (meaning the nerves run in the fatty tissue layer beneath the skin) and/or reconstructing nerves that need to be cut during the mastectomy (meaning they run through the breast tissue and do not stay in the fatty tissue layer). Each person’s situation is unique, so an evaluation to determine if they are a candidate for sensation-preserving mastectomies, as well as if a nipple-sparing mastectomy is right for them and the best choice for their reconstruction, is key to coming up with a final surgical plan. Dr. Anne Peled and her team see patients in-person and through virtual consultation (link to inquiry form) to discuss options and take patients through their surgical journeys.
Why is this procedure so critical and unique?
While mastectomies can be extremely effective at reducing the risk of breast cancer, most women don’t realize that they will have little, if any, sensation in their breast skin or nipple skin afterwards. Because of the way the nerves to the breast skin and nipple travel through the breast tissue, traditional mastectomies tend to cut through these nerves, which leads to breast and nipple numbness for many women, or even sometimes painful sensations at the cut nerve ends. Studies that have looked at sensation after traditional mastectomy consistently show that the majority of women do not ever regain even sensation to light touch throughout their breasts (let alone any pleasurable sensation). Because of the variable nerve anatomy in the breasts, there are some women who may get lucky and have sensation return over time without active preservation of nerves during surgery, but most women will not. With sensation-preserving mastectomy, women are given the opportunity to feel like themselves again after mastectomy without a constant reminder of their surgery as a result of chest numbness.
Dr. Anne Peled has the unique dual training of breast cancer and plastic/reconstructive surgery, which enables her to perform both the mastectomy and reconstruction surgery, a rare combination of skillsets. This, in conjunction with Dr. Ziv Peled’s expertise in peripheral nerve surgery, allowed them to develop a collaborative approach where Dr. Ziv Peled works to keep as many of the nerves to the breast skin as possible while Dr. Anne Peled is performing the mastectomy. Then, for nerves that are unable to be safely preserved, Dr. Ziv Peled uses nerve grafts to reconstruct the cut nerves and provide sensation to the nipple, while Dr. Anne Peled performs the breast reconstruction.
What are the results?
Drs. Anne and Ziv Peled were the first to publish data about this type of surgery. They have found that over 80% of women have sensation that is similar to what they had before surgery, with many women reporting that they often forget they even had mastectomies and reconstruction surgery because their reconstructed breasts feel so much like their breasts prior to surgery. A sensation-preserving double mastectomy and implant reconstruction takes about three to four hours of surgery, with a one-night hospital or surgery center stay. For recovery after surgery, most women can return to their daily lives and activities within two weeks, with complete recovery in most cases in four to six weeks.
Where can i get this done?
Drs. Anne and Ziv Peled were the first to publish data on this procedure, and have pioneered a technique that is very specific to their unique and combined skill sets. As such, most surgeons are not currently educated or trained in sensation preserving mastectomy. Drs. Anne and Ziv Peled see patients from around the country and internationally through video consultations, so whether or not you are in the San Francisco Bay Area, please feel free to schedule an in-person or virtual consultation to see if this procedure is right for you.
mastectomy considerations
PRESERVING the nipple
A mastectomy may be recommended in several different situations, such as patients with certain breast cancer characteristics or women at high risk for developing breast cancer in the future. Although in the past, mastectomies used to involve removal of most of the chest skin and even the chest muscles, current mastectomy techniques are much less invasive. Most mastectomies performed are either skin-sparing, where all of the breast skin except for the nipple and areola is saved, or nipple-sparing, where all of the breast skin including the nipple and areola skin is saved. When performed with breast reconstruction, these approaches can help make the reconstructed breast look more natural and more like the breast before mastectomy.
what will the incisions look like? WILL there be scarring?
There are four common incision types for nipple-sparing/sensation-preserving mastectomies, all of which allow scars to heal well and fade over time: inframammary fold (underneath the breast), peri-areolar (around part of the areola), lateral (from the side of the areola out towards the side of the breast), and inferior vertical (from the bottom of the areola down towards the bottom of the breast).
Dr. Anne Peled is trained in Stryker’s Hidden Scar technique, where she places the incision for a nipple-sparing mastectomy in a location that is hard to see, making the scar barely visible or invisible when your incision heals.
reconstructive procedures
IMPLANT-BASED RECONSTRUCTION
Breast reconstruction can be classified into two categories: implant reconstruction and flap reconstruction (using your own tissue for breast reconstruction instead of implants). 80-90% of women opt for implant reconstruction because flap reconstruction is a much more invasive type of surgery involving both the breast and the site where the flap is taken from that requires a much longer procedure time and hospitalization, as well as extensive recovery after surgery.
The main benefit of implant-based reconstruction is that no large additional scars outside of the breast are needed and the post-operative recovery is often easier, with a typical two- to four-week recovery period.
Implant-based reconstruction for mastectomy can be done in either one stage, where a permanent implant is placed at the time of mastectomy, or in two stages, where a temporary implant called an expander is placed at the first stage and switched to a permanent implant at the second stage. The decision on which approach to use is based on pre-mastectomy breast size and shape, patient goals, and intra-operative assessment following mastectomy. Implant-based reconstruction may also include fat grafting at the second stage of reconstruction in order to help give the most natural appearance of the breast following reconstruction.
direct-to-implant reconstruction
As implant-based breast reconstruction has evolved, two-stage reconstruction with an initial expander is no longer is often no longer necessary. Many plastic surgeons are now realizing that selected patients may be able to have one-stage surgery with an implant placed at the time of mastectomy, which is known as direct-to-implant reconstruction or a “One and Done” approach. The benefits of this approach are that women can avoid the need for a second surgery for the exchange and get to their final reconstructive outcome more quickly.
choosing your implant type
Breast implants can be filled with either saline or silicone. Both silicone and saline implants come in round and teardrop shapes. They also come in different levels of projection across different volumes. Silicone implants have a range of ‘gumminess’, which affects the feel of the implant as well as the shape and how long the implant lasts.
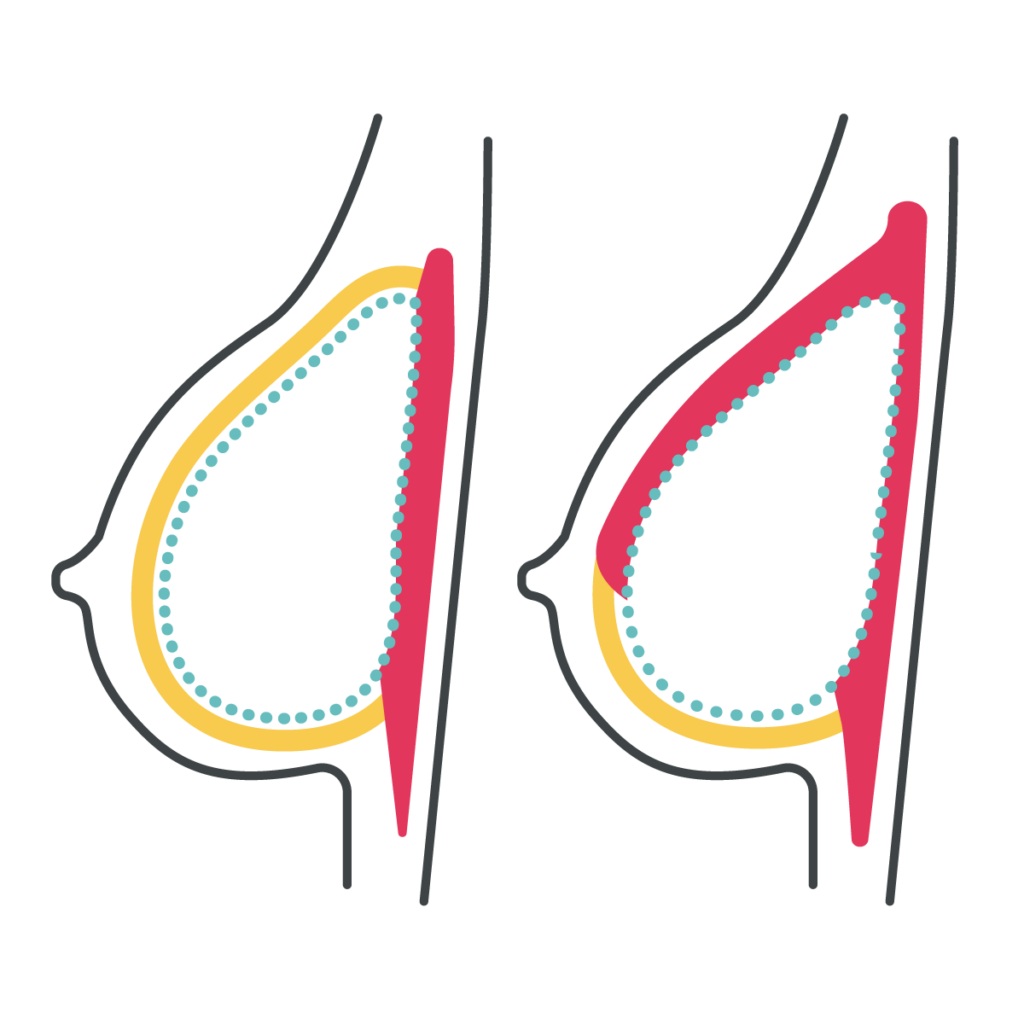
over- or under-the-muscle
Pros: Patients can have a more natural-appearing upper part of the breast, less chronic pain and functional issues from cutting and disconnecting the pectoralis muscle. Patients who have had prior radiation or are expected to have post-mastectomy radiation will also be able to have better shape and symmetry with over-the-muscle implants.
Cons: With over-the-muscle implants, patients may potentially experience more rippling along the top of the breast, and mastectomy skin flap irregularities can be more visible. In addition, some surgeons may not offer this technique depending on their experience and training.
Pros: Under-the-muscle implants are a more familiar technique for many surgeons, based on their prior training. Patients are less likely to have rippling or visible edges of the implant along the top of the breast, and potentially can have better screening for future recurrence if the cancer is right on top of the chest muscle.
Cons: With under-the-muscle implants, patients can experience more short- and long-term pain, and frequently have “hyperanimation deformity” along the top of the breast with pectoralis movement. In addition, the implants are often displaced towards the armpits/sides or appear flattened along the top.
fat grafting
Fat grafting can be done as a part of reconstruction following mastectomy. When fat grafting is used for post-mastectomy reconstruction, it is typically done as part of the second stage of reconstruction, where fat is injected throughout the mastectomy skin flap and sometimes the chest wall muscles to help increase the size of the reconstructed breast and make the shape appear more natural. In both cases, fat grafting entails standard liposuction (typically of the abdomen and/or thighs) in order to obtain fat to use for the reconstruction. The fat is then specially processed in the operating room to get it ready for transfer. After that, it’s carefully transferred back to the breast or mastectomy skin flaps in small amounts throughout the area to prevent lumpy areas within the breast (“fat necrosis”).
sensation preserving mastectomy before & after




in the press
Common Questions
Women who have either been diagnosed with breast cancer or are at high risk for future breast cancer and have elected for mastectomy and implant reconstruction
Depending on the procedure, recovery time can be any time from 2 to 6 weeks.
You can usually start walking within the first week, and can then slowly increase your exercise over next several weeks. You are generally back to full activity in 4 to 6 weeks.
You can find a full list of our favorite products here.
Older generation implants are thought to only last 10 years, but they are anticipating that newer ones will last from 20 to 25 years.
It’s best to consult with a physician to determine if a nipple-sparing mastectomy or sensation-preserving mastectomy is right for you. Not all physicians are educated on the option, so if you’re unsure and you are not in San Francisco, you can schedule a remote consultation with Anne Peled, M.D.
Saline and silicone implants have different benefits depending on the patient. Newer silicone gel implants (a.k.a. “gummy implants”) are commonly used when silicone is selected.
Most women receive smooth implants, but this is always a personalized discussion with each patient.
If you are undergoing a mastectomy, you will not be able to breast feed.
If you are undergoing a mastectomy, you will not be able to breast feed.
Our office has a scar management system that is customized for each patient.
Most people take 1 to 2 weeks off after surgery before they return to work, although that period can be longer if patients have additional/combined procedures involving different parts of their body.